162x Filetype PDF File size 0.34 MB Source: www.royalberkshire.nhs.uk
Wound care nutrition – a resource for patients
Managing and improving wound healing via nutritional interventions.
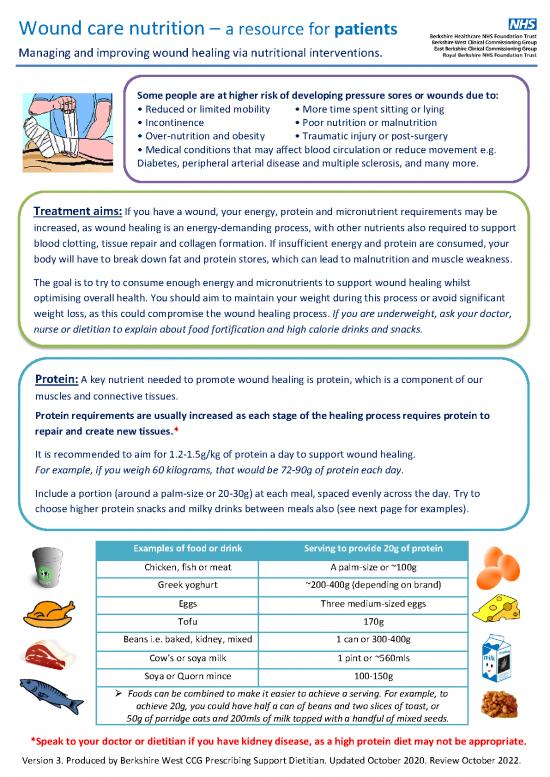
Some people are at higher risk of developing pressure sores or wounds due to:
• Reduced or limited mobility • More time spent sitting or lying
• Incontinence • Poor nutrition or malnutrition
• Over-nutrition and obesity • Traumatic injury or post-surgery
• Medical conditions that may affect blood circulation or reduce movement e.g.
Diabetes, peripheral arterial disease and multiple sclerosis, and many more.
Treatment aims: If you have a wound, your energy, protein and micronutrient requirements may be
increased, as wound healing is an energy-demanding process, with other nutrients also required to support
blood clotting, tissue repair and collagen formation. If insufficient energy and protein are consumed, your
body will have to break down fat and protein stores, which can lead to malnutrition and muscle weakness.
The goal is to try to consume enough energy and micronutrients to support wound healing whilst
optimising overall health. You should aim to maintain your weight during this process or avoid significant
weight loss, as this could compromise the wound healing process. If you are underweight, ask your doctor,
nurse or dietitian to explain about food fortification and high calorie drinks and snacks.
Protein: A key nutrient needed to promote wound healing is protein, which is a component of our
muscles and connective tissues.
Protein requirements are usually increased as each stage of the healing process requires protein to
repair and create new tissues.*
It is recommended to aim for 1.2-1.5g/kg of protein a day to support wound healing.
For example, if you weigh 60 kilograms, that would be 72-90g of protein each day.
Include a portion (around a palm-size or 20-30g) at each meal, spaced evenly across the day. Try to
choose higher protein snacks and milky drinks between meals also (see next page for examples).
Examples of food or drink Serving to provide 20g of protein
Chicken, fish or meat A palm-size or ~100g
Greek yoghurt ~200-400g (depending on brand)
Eggs Three medium-sized eggs
Tofu 170g
Beans i.e. baked, kidney, mixed 1 can or 300-400g
Cow’s or soya milk 1 pint or ~560mls
Soya or Quorn mince 100-150g
Foods can be combined to make it easier to achieve a serving. For example, to
achieve 20g, you could have half a can of beans and two slices of toast, or
50g of porridge oats and 200mls of milk topped with a handful of mixed seeds.
*Speak to your doctor or dietitian if you have kidney disease, as a high protein diet may not be appropriate.
Version 3. Produced by Berkshire West CCG Prescribing Support Dietitian. Updated October 2020. Review October 2022.
Top tips for increasing protein intake:
• Choose higher protein sandwich fillings such as ham, turkey or beef slices, egg, cooked chicken,
tinned fish, cheese or peanut butter.
• Prioritise drinks made from milk, i.e. hot chocolate, milkshakes, Horlicks®, Ovaltine®, milky coffee
or a glass of cold or warm milk.
• Choose higher protein snacks i.e. boiled eggs, omelette, scrambled eggs or beans on toast, cooked
meats, Greek or Skyr® style yoghurts, milk or milkshakes, sandwich with a high protein filling (see above),
nuts, houmous and pitta or vegetable sticks, apple slices with peanut butter or crispbreads and rice cakes
with cottage/cream cheese or quark.
• If you are at risk of malnutrition, you could choose higher energy snacks such as sausage rolls or
cocktail sausages, pork pies, scotch eggs or cheese and crackers. You could also fortify your meals
with skimmed milk powder, whole milk, full fat yoghurt, cheese or ground nuts (if not allergic).
• If you do not need additional calories, choose lower fat and leaner meat and dairy sources.
• Choose milk-based puddings such as yoghurt, rice pudding, custard, semolina or whipped dessert.
• If you follow a vegetarian or vegan diet, choose higher protein meat and milk alternatives such as
Quorn®, tofu and soya. Bulk meals out with beans/lentils or use grains such as quinoa or brown rice.
BALANCED DIET: It is important to consume a wide variety of foods from all of the different food groups
in order to obtain key vitamins, minerals and antioxidants to support optimal healing.
Consume:
• At least 5 brightly coloured fruits and vegetables a day (a portion is about a handful, or a piece of fruit).
• 3 portions of calcium a day, (e.g. 200mls milk, 1 small pot of yoghurt and a small matchbox size of cheese).
• A daily 10ug Vitamin D supplement (all year round for: 65+ years, individuals with darker skin tones, those
who cover up their skin or stay indoors during the day, breastfeeding and pregnant mothers, children aged
1-4 years and all ages in the winter months from October-April).
• 2 portions of fish a week, with 1 portion being oily e.g. salmon, mackerel or sardines.
• Anti-inflammatory fats e.g. nuts, seeds, vegetables oils and avocados and reduce saturated fats such as
cured or fatty meats, cakes, pastries, crisps, chips, butter, lard, and cream (unless trying to gain weight).
• Maximize Vitamin A, C, Iron and Zinc-rich foods: fruit juice, citrus fruits, berries, broccoli, spinach, kale,
peppers, potatoes, eggs, shellfish, lean meat and poultry, fish, milk, cheese, beans, tofu, nuts and lentils.
• And lastly, reduce alcohol intake, avoid smoking and increase physical activity to improve circulation.
Fluid: Fluids help to improve circulation to the skin and prevent Did you know: a large glass of
dehydration. Seeping wounds may lead to increased fluid requirements. milk provides 10g of protein
and a pint contains 20g!
Aim for at least 6-8 cups of fluid a day. If you have a wound, choose
high-protein milky drinks (see above) and higher-energy drinks such as
juices/smoothies if you are underweight. Water, squash, tea, coffee,
soups and juicy fruits all count towards fluid intake. If you want to avoid
weight gain or have diabetes, choose plain milk and limit sugary drinks.
If you need more support with dietary advice for wound healing or weight management, please
speak to your nurse or ask to be referred to a dietitian.
Think, Food First!
Version 3. Produced by Berkshire West CCG Prescribing Support Dietitian. Updated October 2020. Review October 2022.
no reviews yet
Please Login to review.